The following are clarifications of misinformation and answers to frequently asked questions. We have tried to put the answered points into general theme sections. More questions and queries will be answered soon.
Local Housing Developments
We asked for a statement against the housing developments, but the surgery is not willing to offer an opinion. Why?
We recognise that the proposed housing developments are a matter of significant public interest and understandably evoke strong views within the community. However, the practice is not in a position to offer a formal opinion either in support of or opposition to specific developments.
While we have included a section here to outline relevant contextual information as far as we reasonably can, decisions on planning matters fall outside our remit. It is therefore not appropriate for us to issue a statement against the proposed developments.
Some of the objections to housing devlopment are saying the surgery will not cope with extra patients, is this correct?
No!
Concerns have been raised regarding whether the practice can accommodate an increase in patient numbers as a result of new housing developments.
We’d like to clarify that funding for general practice in the UK is directly linked to the number of registered patients. As the population grows, so too does the corresponding funding, enabling us to scale our services accordingly.
Over the past decade, our workload, measured using prescription volumes as a proxy measure, has increased by approximately 25%, despite only a modest rise in our registered patient population. This suggests that the growing demand is largely driven by demographic change, particularly an ageing population with more complex health needs.
The graph below illustrates the disparity between the rising workload and relatively stable population numbers over recent years.
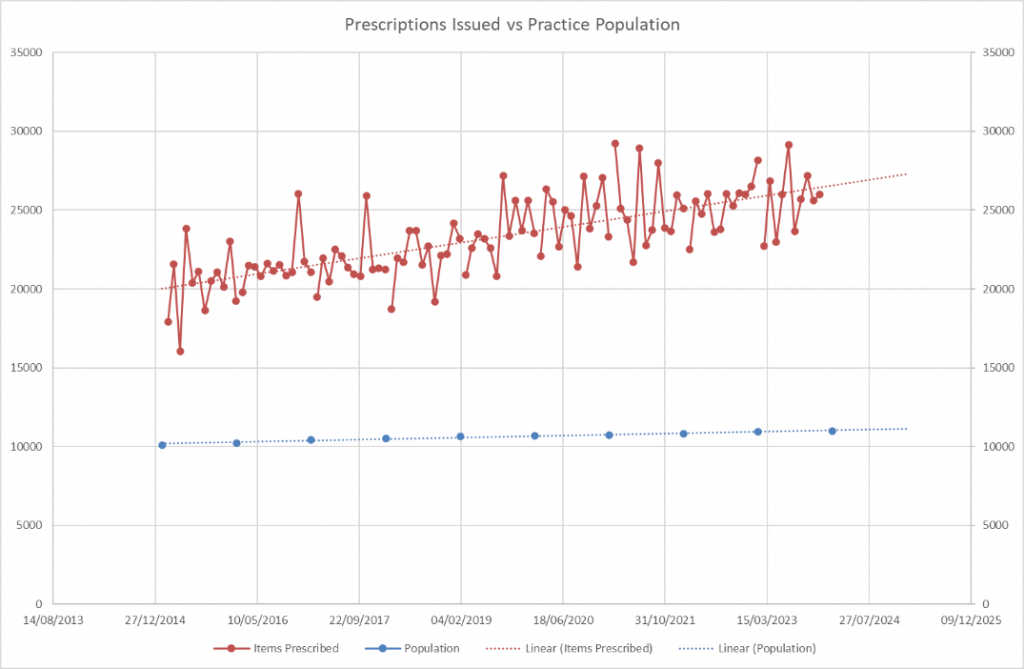
New housing is expected to bring younger residents into the area, potentially rebalancing our demographic profile and helping to alleviate some of the pressures caused by increased clinical demand.
So you suppot the increase in the population in the local villages?
We have outlined how an increase in population has the potential to enhance our ability to deliver care to our patients. While we understand the wider philosophical discussions, such as the notion of ageing communities requiring new “lifeblood”, these lie beyond the scope and remit of our professional contribution to this debate.
What we can say is that, from a service delivery perspective, an influx of younger residents registering with the practice would be beneficial rather than detrimental.
However, we wish to make it clear that we do not, and will not, express any view regarding the specific location or siting of proposed developments.
Appointments
Why can’t I just have an appointment when I call / Why do I have to be triaged?
When you call for an appointment, we use a signposting and triage system to ensure you are seen by the right person, at the right time, and in the right place. This helps us:
- Manage demand fairly – making sure those who need urgent care are prioritised.
- Direct you to the most appropriate clinician – whether that’s a GP, nurse, pharmacist, or another healthcare professional.
- Provide advice when an appointment isn’t needed – saving you time and helping you manage minor issues at home.
This approach ensures everyone gets the care they need as efficiently as possible.
You clearly don’t have enough appointments!
We understand it can feel like there aren’t enough appointments, but our workload data shows otherwise. Each month, we provide around 3,500 appointments with GPs, Advanced Care Practitioners, and similar clinicians—equivalent to a third of our registered population. When we include other appointments, that number rises to over 5,000—half our entire population every month!
This should be more than enough to meet demand, which is why signposting and triage are vital. They ensure patients are directed to the right service, the right person, or the right clinic—helping us manage appointments fairly and efficiently.
Why can’t I book more than 2 weeks ahead?
The government made it a requirement for practices to offer appointments within 2 weeks. This is retrospectively measured by NHS systems by looking at when an appointment was booked, and if it was more than two weeks then that counts as a fail even if it was patient choice. Although you are supposed to be able to mark a flag that says patient choice this does not work. The vast majority of Staffordshire practices (and likely all of England) practices have adopted the same process.
We do not like this requirement, however we must work within it.
Why can’t I book a smear test?
Our new, very qualified and capable nurse, was due to start and overlap with the previous nurse who was leaving. That overlap would have allowed the leaving nurse to sign off the new nurse as competent and that would have a seamless continuation of appointments. The leaving nurse did not remain in post in order to allow this. The new nurse is waiting to be cleared to do smears.
Why does the nurse have to be signed off to do smears, why can’t the doctors do them?
Unfortunately, the push for regulation (some may say over regulation) of aspects of healthcare require healthcare workers to undergo specific training and then obtain a PIN number that allows a smear taken by them to be processed. This is a national requirement. Most doctors will not do enough smears in a year to maintain their accreditation and therefore, no doctors are allowed to take smears. This is the inevitable consequences of how healthcare services are being managed/regulated.
Hot off the Press 03/02/2025:
Our second experienced, senior nurse has now started. Both nurses are now signed up and ready to do smears. You should be receiving links soon to book in.
About time – I’ve been waiting over a year!
We do not understand why you haven’t been able to book in but want to explore and learn from why you’ve been unable to book. The only period when we had no availability for smear tests was from 23rd December 2024 to 4th February 2025—just over a month.
If you’ve experienced difficulties booking for a longer period, we would really appreciate your feedback to help us identify any issues. We will soon be releasing a survey to gather insights on this, and your input would be invaluable in improving our understanding of what stopped people booking in for over a year. [14/04/24 update: after informal feedback it would seem there was no real reason for the alarm and patients were able to book other than the very short period mentioned above. We will therefore not be running the survey. However, if you have feedback about why you were unable to get an appointment outside the dates above please contact the ppg on feedback@brewoodppg.co.uk]
Thank you for your patience, and we encourage you to get in touch if you’re still struggling to book an appointment.
Why can’t I get a blood test appointment at the surgery?
We understand your frustration and appreciate your patience. Unfortunately, a combination of staffing challenges has led to a backlog of blood test appointments at the surgery.
Several key staff members, including nurses and Health Care Assistants, left for various reasons. While we cannot discuss individual cases due to legal reasons, these departures, combined with employment law restrictions on advertising certain roles while staff were on sick leave, made recruitment more difficult. Additionally, recruiting for these roles takes time, as it involves various checks and references before new staff can start. Some newly recruited staff also withdrew before starting or left shortly after joining, adding to the delays.
However, we have been actively addressing this issue. We now have two Health Care Assistants, a Phlebotomist, and two new Nurses. As our new team gets up to speed, the availability of blood test appointments should improve.
If I walk out after waiting for an appointment does this count towards missed appointments?
No. Walk-outs count as walk-outs and not as missed appointments. These are by definition two different things.
Why have people had to wait so long that they had to walk-out.
We understand that waiting longer than expected can be frustrating, and we sincerely appreciate your patience. No clinician is deliberately running late—when delays occur, they often result in clinicians working later into the day to ensure all patients receive the care they need.
There is a necessary balance between keeping to schedule and giving patients the time their concerns require. In a busy NHS general practice, this balance is not always perfectly achievable. Clinicians frequently run late due to complex patient needs, medical emergencies, or other unforeseen factors.
We acknowledge that this can be inconvenient, but we are grateful that most of our patients appreciate the challenges we face. Your understanding and support help us continue to provide high-quality care to all who need it.
Telephones and Call Backs
I have requested a call back but no one has called me back yet!
Call backs continue to be made throughout the day. They hold your position in the queue and you will get a call when your place in the queue comes up. If it is taking a long time, it is likely there were a lot of calls before indicating the huge demand on our non-emergency service. If you have an emergency problem you must call 999. Please wait for your call back which could occur later in the day.
Please ensure you have signal on your phone and are able to answer the call during the course of the day as your turn in the queue could come up at any time.
We generally try to call back at least twice. If you have missed calls or did not have signal when called, you may need to call back and re-log your call. The use of the online eConsult system allows you to submit a query directly onto a list and will get you advice or a call back – it also means that if you miss calls then the eConsult will not be completed until enough attempts have been to contact you, and the information provided allows a better judgment as to how we should contact you. You can access eConsult here.
If you have waited all day and you have not had a call back, then please check for missed calls and answerphone messages. If you have not had a call back at all then there may have been an error, please call back. Powercuts can affect call backs, failures in the cloud telephony platform can also cause failed call backs, failures in internet connectivity can also cause failures of call backs – these are out of our control, but we apologise for the inconvenience. Please accept our apologies and re-log your call back the following day. If you have an emergency request please call 999 as we do not cover emergencies.
I am being asked to enter a PIN when I call in but I don’t have one. How do I get a PIN?
You are asked to set up a PIN the first time you call and use the automated system. It is important to remember this PIN or store it in a secure way so you can find it if you forget it. If you are being asked for a PIN, you will have set one up when you first called in to the automated system. To get a new PIN we will need to set a new one for you. We need to ensure that the person asking for a new PIN is in fact the patient, hence the need to check ID. We apologise for the inconvenience this may cause but we have to do this to safeguard your confidentiality from the risk of unauthorised people trying to access your account. If you require a new PIN please contact our team via email to the main practice email and they will provide further instructions or alternatively, please attend the surgery with photographic ID (such as a passport or photo driving licence) and the team will assist you.
I have forgotten my PIN for the automated phone system, how do I reset it?
To get a new PIN we will need to set a new one for you. We need to ensure that the person asking for a new PIN is in fact the patient, hence the need to check ID. We apologise for the inconvenience this may cause but we have to do this to safeguard your confidentiality from the risk of unauthorised people trying to access your account. If you require a new PIN please contact our team via email to the main practice email and they will provide further instructions or alternatively, please attend the surgery with photographic ID (such as a passport or photo driving licence) and the team will assist you.
I keep getting cut off on the automated phone system or get the message “thank you for calling, goodbye”
We need your help to improve this system. If this happens to you, please record the time of the call and the number you called from. We can then let the system provider know and ask them to look into the reasons why that is happeneing. Without your help, we cannot give the provider the information they need to find what causes glitches and fix them.
The provider has been in this market since 1991 and is a well established provider. They have worked with practices since 2003. We are not sure why glitches occur in such a well established system but when they do, we need the information to help improve it.
The phone system is now automated, how do I get to actually speak to someone?
The option to sleect the traditional menu still exists. If you listen to the message, it will tell you which option to select for the traditional menu. The automated menu is able to handle most queries – please listen to all the options and information. We understand people want to quickly navigate menus but we also would like patients to avoid queues waiting to speak to someone when you can access what you need more efficiently. However, if you choose the traditional menu you may have a wait before your call is answered.
I waited in the phone queue only to be cut off!
We are sorry to hear that, however, we have experienced some issues with the phone systems. The phone system is from a large cloud based telephony (CBT) provider, we understand glitches can occur. We are not technically knowledgeable enough fully to understand how Cloud Based Telephony works but we understand your call is held in “the cloud” and transferred to our lines once your call is ready to be answered. Your call could be dropped by a glitch or limitation in your phone line, a problem or glitch in the CBT provider’s systems, or an issue at the local BT exchange, or a local issue with our internet connection, or a variety of other issues. We do not own these providers and we have not built the systems and we are just as frustrated by glitches and errors like these as you. Please let us have the details of what time you called, what phone number you called from, what phone menu options you chose and any other information you have so that we can give this information to the relevant provider and ask them to look into and prevent similar recurrences.
Records, Prescriptions, Letters, Referrals etc
Did you really lose someone’s records for 3 years?
No! Whilst we cannot discuss details of a claim about this on social media – this is a lie. Without full written permission to divulge the information online in public, we are unable to tell the truth. Furthermore, even if we were given permission to do so, it would likely not be in anyones interest to divulge the information, nor is it likely to be supported by the ICB or our indemnity organisations.
Nonethless, by way of a generic explanation, when a patient registers, we send a request to Primary Care Support England (PCSE) for the records to be transferred. Electronic records transfer electronically and any paper records are sent to us – we have no control over how long it takes PCSE to locate and send those records.
I forgot to order my medication on time. I need it urgently as I have run out of my important medication!
We need around 72 working hours (9am-5pm) in order to process prescription requests. If you need an emergency supply of medication, please call 111 for the emergency prescription service or use the online tool here.
I have ordered a repeat prescription, how long will it take?
We try to complete requests in around 72 working hours (9am-5pm) in order to process prescription requests. Saturday and Sunday are not working days. The process only starts from when we recieve the request not when you hand it to your pharamcy. Certain things may delay your request such as queries about medication or if you are due a medication review. If a request is submitted at 6:30pm on a Friday it will not be seen by us until 9am on Monday for the start of the 72 working hours. We apologise for the occasisions where the prescriptions take longer than the 72 working hours – there are various possible reasons, we do try to avoid delays, and do look at why delays occur when they do to try to learn from them.
Why does it take so long to get a prescription?
Signing a prescription in general practice can take time due to several factors. Clinicians must review each request carefully to ensure the medication is appropriate, safe, and in line with clinical guidelines. This includes checking for drug interactions, contraindications, and patient history. Repeat prescriptions may also require periodic medication reviews to confirm ongoing suitability.
Clinicians manage high workloads, balancing patient consultations, referrals, and administrative tasks. Prescription signing is often done in batches between other duties, which can cause delays. Electronic prescriptions, processed via the NHS Electronic Prescription Service (EPS), can sometimes experience technical issues or require additional verification.
Certain medications, such as controlled drugs, demand stricter checks and legal compliance, adding to processing time. If a prescription raises concerns—such as an unusual dose or missing details—the clinician may need to contact the patient or pharmacist for clarification. Urgent prescriptions are prioritised, but routine ones may take longer, depending on workload and complexity.
The above has to be considered for every prescription to a lesser or greater extent; unfortunately it is not as simple as just signing a presciption like it used to be in the days of paper prescriptions from 15-20 years ago, but it is much safer!
Staffing
Why don’t you just employ more people?
Staffing numbers are higher than ever. Our staff car park had enough spaces to accommodate the staff we had with spaces to spare when we opened the new surgery, but now there are not enough spaces to fit all the staff – this in itself shows the growth in staffing numbers.
Why is there such a high staff turnover?
We were asked for information on staff turnover in October 2024 and we responded with:
“This would be a difficult percentage to have accurately, given some staff are full time and some part time. However, in the past 12 months, we have had 59 people working at the surgery. 12 people left (not including those dismissed or retired). That is 20%. We understand the average UK staff turnover on ‘Healthcare and education’ is 20-25%. In fact, according to NHS Digital data, the turnover is around 30%. Further information is provided in the attached document for detail.”
We will look staff turnover rates again in due course and will update the information.
Why did the Health Care Assistants/Phlebotomists leave?
Unfortunately, we cannot discuss the reasons why members of staff are no longer employed. However, we now have highly qualified staff in place who have a wider range of skills and knowledge and are able to do more for our patients.
I have seen posts or heard comments from ex-staff that there are problems at the practice?
Any unsubstantiated claims by disgruntled ex-employees should be considered with caution and disregarded without supporting examples or evidence. People should consider whether disgruntled ex or leaving employees provide accurate testimonies. Caution must be taken to not implicate yourself in slanderous behaviour.
We have also been made aware that some patients have told new team members that previous staff have claimed there are problems between staff or that this is not a good place to work. These statements are untrue and should not be spread.
It is difficult to understand why anyone would deliberately try to undermine the practice based on the views of a disgruntled ex-employee. Comments like these can unfairly influence new staff, leading them to perceive issues where none exist. This, in turn, can make them feel unsettled and more likely to leave, reducing our capacity and causing further staffing issues.
We kindly ask that any attempts by ex-employees to undermine the practice are kept away from new staff. If patients have specific concerns they wish to raise, they should do so through the Patient Participation Group (PPG).
I think all the staff are overwhelmed and have too much pressure put on them! Is that why they leave?
We recognise that there is a significant amount of pressure on the practice and those delivering services. This pressure predominantly stems from patients, bureaucracy, and various demands. Given this unprecedented pressure, we have to balance the workload expected from staff with their free time, as this directly impacts patient access. If staff had no work, they wouldn’t feel pressure, but that would also mean no patient access. Our staff work very hard, often continuously. Most staff understand that this is the nature of working in general practice, particularly in a high-demand patient population like ours. However, some may not feel they should work continuously. Such staff may not stay long or might not pass the probationary period due to this. Additionally, staff need to perform their jobs effectively and efficiently. In the modern world, it’s increasingly difficult to ‘carry’ staff who aren’t able to perform, as it affects patient care, access, and the staff morale of others.
Other, uncategorised concerns or queries
Why do you make excuses for the problems?
If we try to explain the difficulties, they are called excuses. If we show data that proves a point, the naysayers claim the data is incorrect. If a patient tells a lie, we cannot correct it due to confidentiality.
Where concerns and issues are raised through the correct channels (PPG or Complaints) and are found to be valid, we do take them seriously and act on them. However, unfounded, sensationalised, and half-truths on social media serve only to feed the egos and desire for self aggrandisement of certain individuals, while simultaneously adversely affecting staff morale and reducing the pool of potential applicants to available posts.
What we offer is not excuses, but explanations, which is something that certain types of individuals are not able to accept – that is a reflection of them and not the validity of the explanation.
Why is Dr Ahmed buying the Pink House?
Dr Ahmed is unaware of why or if he is buying the pink house, there are rumours of a private hospital and of an asylum seekers refuge. We have even heard that he intends to turn it in to a housing developement of 40 houses. We approached Dr Ahmed for comment but he burst into laughter and was unable to speak anymore. We will ask again in the hope he gives us an answer.
Dr Ahmed was overheard in the corridor speaking to a local councillor about putting in a planning application for an adult services facility. The councillor seemed agreeable. We believe this was joking banter but need to investigate further.
Funding
I read a post that says you get £170 a patient, so I am entitled to lots of appointments!
We believe this figure is wrong and does not relate to Brewood Medical Practice. The post in question, we believe was posted by an employee of Price Waterhouse Cooper (PWC). PWC has had hundreds of millions of pounds of NHS funds to provide managment support.
Here are some facts:
Our patient list is around 11,000 – based on our General Medical Services funding we get around £160 per patient.
Our weighted list size (one that attempts to calculate what our demographics represent in real terms demand) is around 12,500 – based on this it is around £142 per patient.
£160 has to cover the administration for every registered patient’s records, respond to Integrated Care Board/NHS England requests for any information, securely store the information, curate records, manage the patient’s NHS registration – clearly this has a cost. We would argue that if that service was purchased from PWC, it would cost a lot more. An annual streaming service subscription, or several months of a mobile phone contract – whether you use the service or not, costs more than this. In addition to all the above, we have to provide appointments to the population registered. It is not an individual person’s allocation – it is an overall global sum for the number of patients registered – the number of patients being a reflection of how much funding a practice should receive as a share of the national allocation.
Some disingenuous people, and we are by no means suggesting any particular individual is disingenuous, picking information to push a narrative of overpaid general practice is despicable and clearly aimed at trying to contribute to the ongoing negativity and hatred towards general practice – of which it seems that Brewood Medical Practice has more than it’s fair share.
Coven Memorial Hall
There is now a set of dedicated pages relating to Coven Memorial Hall here.
Will the Medical Room in Coven open again?
As of January 2025, we are waiting for the Integrated Care Board (ICB) to conduct a feedback exercise and look at what the need in Coven for a facility is. Once they have undertaken this exercise, we will be in a better position to understand what is needed and what can be provided. We will then need to understand what Coven Memorial Hall are able to do to bring the room/facility up to the required standard.
Coven Surgery: Setting the Record Straight
11th November 2025
Coven Surgery: Setting the Record Straight, Including and an Open Request to the Trustees of the Coven Memorial Hall
Brewood Medical Practice wishes to clarify its position following statements recorded in recent PPG minutes concerning the reinstatement of a surgery in Coven.
We remain fully committed to restoring healthcare provision in Coven. Any new or reinstated facility, however, must be safe, sustainable, and compliant with NHS and CQC standards.
Background and Current Situation
For several months, the Practice has sought to work collaboratively with the Trustees of Coven Memorial Hall to identify a viable route forward. Unfortunately, despite repeated efforts, the Trustees have not been willing to bring the existing rooms up to the required clinical standard. The space continues to fall short of infection control and safety requirements, which prevents its lawful or safe use for NHS care.
The Practice therefore proposed a practical alternative: the siting of a modular building (Portakabin-type unit) on an area of hard standing within the Hall grounds. This would have been fully funded by the partners of the Practice, with no cost to the public for the purchase or siting of the structures. However, the Trustees declined this reasonable proposal and instead offered a strip of land beside the brook, an area unsuitable for construction due to waterlogging and subsidence risk.
Furthermore, the Trustees proposed a seven-year lease, which provides no long-term security. When this concern was raised, one of the Trustees replied that the Practice could simply “take the building with you” at the end of the term. This comment demonstrates the difficulty the partners have faced in trying to agree fair and sustainable terms for the benefit of Coven patients.
It should also be noted that, even whilst the medical rooms at Coven Memorial Hall have been out of use, the Hall has continued to receive rental payments above the NHS valuation for the space. These additional payments have been personally subsidised by the partners of the Practice, in good faith and in support of maintaining a presence in Coven. Those funds could reasonably be reinvested by the Trustees to bring the facility up to the required standard.
Practice’s Position
Brewood Medical Practice remains willing and eager to provide services in Coven. The partners continue to support the modular building solution, which is the quickest, safest, and most cost-effective way to restore care locally.
Given the Trustees’ apparent reluctance to permit this on suitable hardstanding, the partners are now exploring an alternative configuration that could utilise the grass area in front of the Memorial Hall. This would comprise a modular Portakabin for clinical rooms and a lightweight adjoining structure to act as the reception and waiting area. This approach could be installed with minimal disruption and removed if necessary, ensuring flexibility and full reversibility.
The partners will shortly be writing formally to the Trustees with this proposal.
Rebutting Mischaracterisations
It has been suggested in public records that the Practice, or Dr Ahmed personally, has been difficult to deal with. This is untrue. The difficulty arises only because the proposals offered so far have been impractical, non-compliant, or commercially unviable. The Practice has remained courteous, transparent, and focused on solutions throughout, seeking only to secure safe and sustainable healthcare provision for Coven residents.
Next Steps
We call upon the Trustees to re-engage constructively, either by:
- Bringing the existing premises up to full regulatory standard, or
- Agreeing reasonable lease terms and site use for a modular facility.
The partners of Brewood Medical Practice stand ready to progress either option without delay, in partnership with the ICB and other stakeholders. Our only objective is to see Coven patients once again receive the accessible, high-quality care they deserve.
Proper Channels, Facebook, Social Media, Vigilante actions
Why did you publicly name some people who went through the proper channels?
This relates to the individuals who conducted a biased survey about an organisation that does not exist, they were very vocal on social media (not the correct channels). They refused to engage with the Patient Participation Group (i.e. refused to follow the proper channels). They contacted the Care Quality Commission (CQC) with an untrue claim that the CQC felt obliged to investigate. They then placed a Facebook post making clear they had instigated the investigation – they chose to publicise their actions on social media for a prolonged period. They subsequently made clear to us that they “went to the CQC” because Dr Ahmed refused to meet with them about the survey data they had collected – data that has never officially been sent to us by them, nor sent to the PPG, nor published. Summoning a GP to a public meeting or demanding to have a meeting with a GP about an unsanctioned, improper survey “or else”, is unprecedented and totally inappropriate. Names of these individuals was already in the public domain, they had already, themselves, made clear what they had done, they had not gone through any proper channels and raised an untrue complaint with the CQC because Dr Ahmed didn’t meet with them about their survey about an organisation that does not exist – none of this is proper.
These individuals did not go through proper channels and raised a CQC complaint out of spite (as they admitted themselves). Therefore, mentioning the username of the poster of the Facebook posts and mentioning the names from social media was not naming any individuals, it was naming Facebook accounts and names taken only from Facebook – Facebook is not a proper channel. Individuals were not named from any official channel – only from improper channels.
Onine access
I can’t view my records on the NHS app, how do I get access?
Access to records is activated at our surgery. You use you NHS app to gain access using your own personal details. We do not have any additional access or ways to enable access for you. You can visit https://www.nhs.uk/nhs-app/ for lots of information that may help.
Information on getting started with the NHS App is here.
You can find contact information for the NHS App team here.
Brewood Surgery
The speaker volume is very loud at the desk when talking to the receptionist, everyone can hear!
We are sorry that the screens have remained in place, making the speaker neccessary. There are a number of options to speak to a member of the team at the desk. You can use the two way phone which provides more privacy. The open waiting area is a common arrangment in many GP surgeries and hospital outpatient departments – We have tried to reduce the volume on the speaker but it is then too quiet for some patients. If it is too loud please ask the receptionist to turn the volume down.
We will look at adding holes to the screens and reducing their height in the comming months to see if we can remove the need for the speaker. We thank you for your patience on this matter as it has taken longer than we had hoped.
Why can’t the screen in reception be taken down now?
There a few reasons why the screens remained in place, despite having intended to taken them down some time ago. We found that the screens have provided an infection barrier for the staff. There has been increasing hostility towards the staff and the screens provided some protection. We have been looking for effective alterantives but unfortunately other matters have taken priority. We apologise that we have not been able to allocate the time needed to look at the screens issue but we hope to make some progress after the winter period and hope to have some plans by mid 2025.